What is diabetes?
Find important information about type 1 and type 2 diabetes and get connected to personalized support.

Type 1 diabetes (T1D)
An autoimmune disorder where your body makes little or no insulin because your immune system has attacked insulin-producing cells in your pancreas.
5% to 10% of adults with diabetes have type 1.
Treatments must include long-acting (basal) and mealtime (bolus) insulin therapy.

Type 2 diabetes (T2D)
A metabolic disorder that prevents your body from producing enough insulin and also makes your body more resistant to the insulin that is produced.
90% to 95% of adults with diabetes have type 2.
Treatments may include insulin.
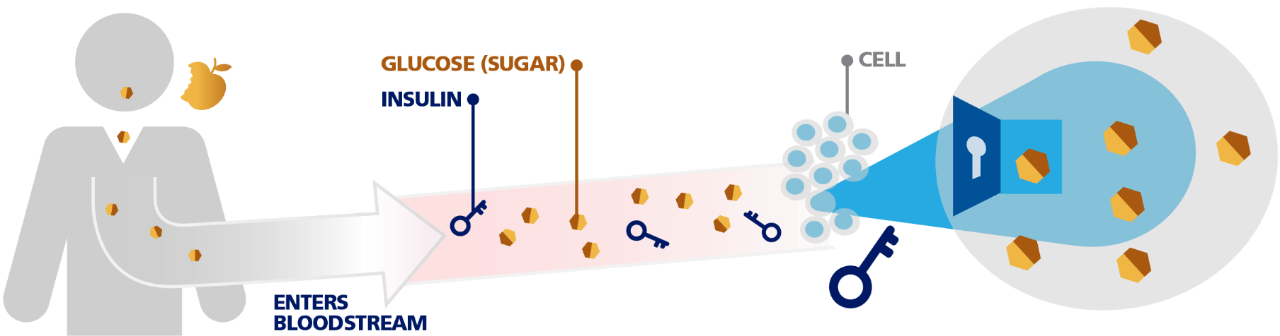
How Food, Sugar, and Insulin Work in the Body
Your body breaks down certain foods you eat into a type of sugar called glucose.
This sugar (glucose) enters your bloodstream and travels to different cells in your body.
Insulin acts like a key, opening the cells in order to let the sugar move out of your blood and go into your cells. The sugar is then used by your cells for energy.
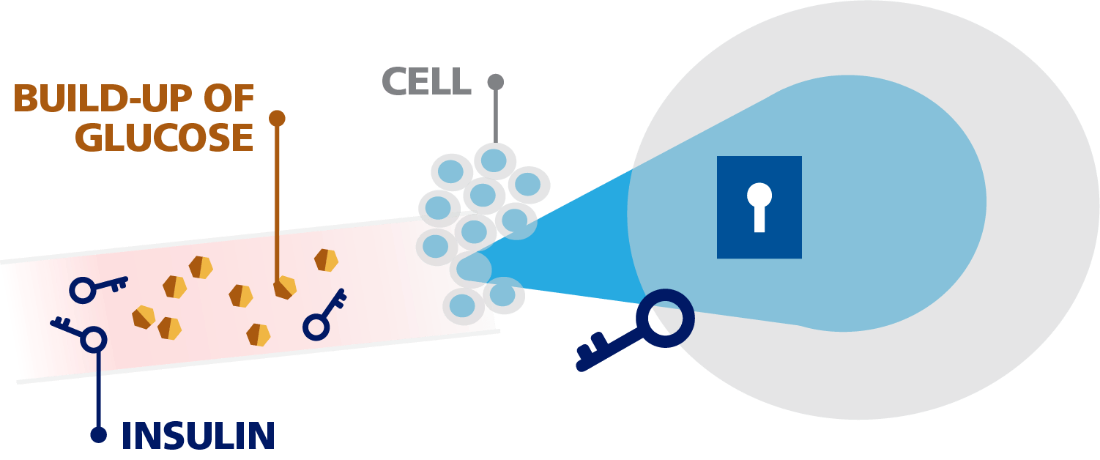
How Diabetes Affects the Body
Diabetes occurs when the body does not make enough insulin or doesn't respond to insulin properly. Without insulin, sugar builds up in the blood, causing high blood sugar. High blood sugar can lead to other health problems.
Why insulin?
Depending on what type of diabetes you have and how much your diabetes has progressed, your health care provider may recommend insulin to better control your blood sugar levels and lower your A1C. If you have diabetes, it’s important to know that even if you’re following your treatment plan, your diabetes can change over time. Your health care provider will work with you to develop a plan that works best for your needs.
You can take insulin by subcutaneous injection (with a pen or vial and syringe), or inhalation or with a continuous subcutaneous infusion via an insulin pump.
Long-acting insulin vs rapid-acting insulin
Different kinds of insulin work for different lengths of time:
Long-acting (basal) insulin lowers blood sugar throughout the day and may be taken to manage blood sugar for many hours and overnight.
Rapid-acting (bolus) insulin, also called mealtime insulin, helps control your blood sugar when taken as prescribed.
How do these 2 types of insulins work together?
Bodies usually release insulin:
- In a steady “basal” amount throughout the day and night
- In “bolus” bursts to control blood sugar spikes when you eat
Basal-bolus therapy is the combination of long-acting insulin with short-acting or rapid-acting insulin, which more closely mimics how the body’s natural insulin works throughout the day.
Is this your first time injecting?
You may have concerns about adding an injectable medicine to your daily diabetes care plan. Once you gain a little practice, injections can become part of your daily routine. If you have questions about how to inject your insulin, be sure to talk to your health care provider or someone on your diabetes care team.
Watch a video to get step-by-step instructions on how to inject your insulin properly.
Understanding low blood sugar
The goal of any diabetes treatment is to lower blood sugar. However, it is possible for your blood sugar to drop too low. Ask your health care provider what blood sugar level is considered low for you.
If you are taking insulin, you should know the symptoms of low blood sugar (also called hypoglycemia):
- Sweaty
- Hungry
- Confused
- Shaky
- Lightheaded
- Dizzy
- Sleepy
- Nervous
These are not all the possible symptoms of low blood sugar. Talk to your health care provider to get a complete list of symptoms.
Severe low blood sugar
If these symptoms go untreated, low blood sugar can become severe. People having a severe low blood sugar episode (or severe hypoglycemia) may require assistance from another person for recovery. Severe low blood sugar may lead to seizures and loss of consciousness.