Welcome to your Tresiba® Starter Kit
If your health care provider prescribed Tresiba® to help manage your diabetes, you're in the right place. Below you'll find the information you need to get started on Tresiba®.
Let’s get you started
Your health care provider may have prescribed you Tresiba®, a once-daily, long-acting insulin that manages blood sugar for 24 hours for powerful A1C reduction. Once injected, insulin helps the sugar in your blood get into your cells, providing those cells with the energy needed to fuel your body. One of the things that makes Tresiba® different from other long-acting insulins is the slow and steady release that works the way the body’s insulin does.
For adults, any-time-of-day dosing means you don’t have to worry if you miss a dose of insulin
If you miss a dose of Tresiba®, you have options! Adults with type 2 diabetes can take once-daily Tresiba® at any time of day, if needed. It’s best to take Tresiba® at the same time every day, but if you miss or delay your regular daily dose, take Tresiba® as soon as you remember, then continue with your regular dosing schedule. Just make sure to leave at least 8 hours between doses.
Important Things to Remember as You Get Started
Using your insulin pen
Discover the resources below to help you become comfortable with your Tresiba® FlexTouch®. Before you know it, injecting will become another part of your daily routine!
- Read the Instructions for Use for details on how to take Tresiba®
- Call 1-877-246-8910 to talk to a Tresiba® FlexTouch® Pen Specialist from 9 AM to 6 PM ET, Monday to Friday (excluding holidays) for a free, one-on-one, live training session
- Watch a step-by-step video to learn how to use your Tresiba® FlexTouch®
Storing Tresiba® FlexTouch® and vialsa
Storage before useb

Store unused Tresiba® FlexTouch® pens and vials in the refrigerator at 36°F to 46°F (2°C to 8°C)
Storage after use (8 weeks)c
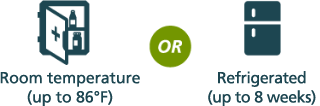
Keep at room temperature (up to 86°F) or refrigerated for up to 8 weeks
aDo not freeze Tresiba®. Do not use Tresiba® if it has been frozen.
bUnused pens and vials may be used until the expiration date printed on the label if kept in the refrigerator.
cKeep away from direct heat and light.

Hypoglycemia—what to watch out for
When you’re taking insulin, you need to look out for low blood sugar, or hypoglycemia.
- Ask your health care provider what blood sugar level is considered low for you
- Be aware of some of the symptoms of hypoglycemia, such as feeling sweaty, hungry, shaky, lightheaded, or dizzy
- Get to know all the symptoms of low blood sugar. Download a fact sheet »
Why tracking blood sugar matters
Checking and tracking your blood sugar helps you and your health care provider monitor how Tresiba® is working. Learn about some options to keep track of your blood sugar:
- Talk to your health care provider about a continuous glucose monitoring (CGM) system
- Keep track of your blood sugar with a blood sugar diary

Personalized support for diabetes
There’s no need to manage diabetes on your own when you have the support of a NovoCare® Diabetes Health Coach at no cost! Your Health Coach can help answer your questions one-on-one, provide healthy eating ideas and tips to help you stay strong, as well as help you stay motivated to set and reach your goals.

We understand how important it is to have access to the insulin you need to manage your diabetes. Novo Nordisk has affordability programs for every insurance situation in order to provide support for those who need help.
Type 2 Diabetes
Questions to Ask Your Health Care Provider About Tresiba®
Always consult your health care provider when starting a new treatment or making changes to your meal plan and activity levels. It is also important to ask questions as you continue taking Tresiba®.

What is my target blood sugar range and when should I be checking my blood sugar?

What is my starting dose of Tresiba® and how should I adjust my dose?

What should I do if my blood sugar goes too low?
Type 1 Diabetes
Questions to Ask Your Health Care Provider About Tresiba®
Any time you make a change to your treatment plan, like starting on an insulin such as Tresiba®, you should have a conversation with your health care provider. This is important as you continue taking Tresiba® as well.

What is my target blood sugar range and when should I be checking my blood sugar?

What is my starting dose of Tresiba® and how should I adjust my dose?

What should I do if my blood sugar goes too low?
